Humans take more than 20,000 breaths every day, but most people don't really understand what their lungs are doing during each of those breaths. As air pollution increases, the incidence of chronic lung diseases such as asthma, COPD, and pulmonary fibrosis is rapidly escalating.
The lungs not only sustain life, but are also the starting point for all energy cycles in the body. Any abnormality in respiratory function leads to systemic disorders.
A correct understanding of lung function is the foundation for disease prevention, early detection of damage, and optimization of long-term quality of life.
For a full breakdown of lung anatomy, see "how your lungs are structured"
Your lungs deliver oxygen and remove carbon dioxide during every breath.
Basic Overview: What Is the Function of the Lungs?
The lungs are more than just air-holding organs—they are the life-coordinating centers where each breath carries oxygen to nourish each cell and simultaneously removes carbon dioxide—a dangerous waste product produced by metabolism. Inside the chest, the two lungs operate continuously, in harmony with the heart and blood vessels, to ensure optimal airflow. This process is silent but is the foundation for all life activities.
Oxygen intake
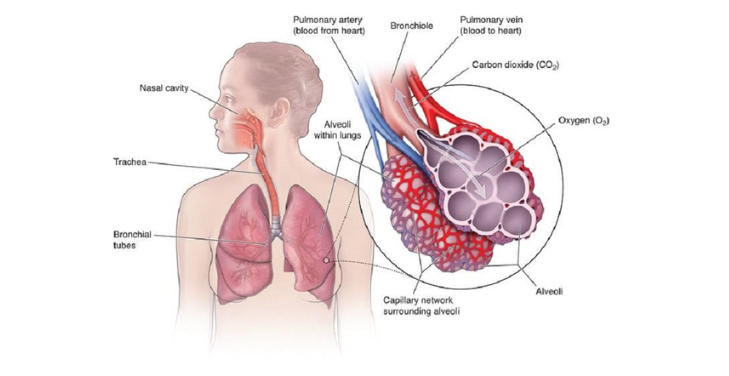
Air enters the nose, passes through the trachea, divides into two main bronchi, passes through millions of small air tubes, and ends at the alveoli. Here, oxygen diffuses into the pulmonary capillaries, where the journey to each cell begins.
Carbon dioxide excretion
At the same time, CO₂ – a waste product from the cells – moves in the opposite direction, from the blood into the alveoli. When you exhale, your body thoroughly removes CO₂ from your circulation, maintaining homeostasis and a stable pH in your blood.
The Mechanics of Breathing: Inhalation and Exhalation
Breathing is more than just moving air in and out of the body – it is a precise physiological process, controlled by pressure, volume, and the mechanical action of many muscle groups. Each breath results from a coordinated effort between the diaphragm, intercostal muscles, and structures in the chest. The human body adjusts its breathing rhythm flexibly, responding to changing oxygen needs from moment to moment.
Inhalation – when negative pressure is created
When the diaphragm contracts and the external intercostal muscles lift the chest, the chest cavity volume increases markedly. This expansion creates negative lung pressure, causing oxygen-rich air to quickly flow through the airways.
Exhalation – when elasticity pushes air out
During exhalation, the diaphragm relaxes, the intercostal muscles lower, and the chest returns to rest. At this point, the lungs contract using natural elastic force, pushing CO₂ out. The entire cycle repeats thousands of times every day to maintain continuous life.
Gas Exchange in the Alveoli
The alveoli are the final functional units of the respiratory system, where vital gas exchange between air and blood occurs. With a grape-like structure, each lung contains hundreds of millions of alveoli, creating an exchange surface of up to 70 square meters. Here, the boundary between gas and blood is only as thin as a layer of cells, enough for oxygen and carbon dioxide to diffuse effectively in every biological second.
Oxygen diffuses into the capillaries
When oxygen-rich air reaches the alveoli, the oxygen concentration is higher than in the surrounding capillaries. The concentration difference promotes oxygen to pass through the alveolar-capillary membrane, dissolve into the plasma, and bind to hemoglobin in red blood cells.
CO₂ leaves the blood and returns to the alveoli
At the same time, CO₂ gas – a waste product of cellular respiration – moves from the blood into the alveoli by simple diffusion. When you exhale, CO₂ is pushed out of your body, completing a delicate and continuous gas exchange cycle.
Transporting Oxygen and Removing Carbon Dioxide
After gas exchange in the alveoli, gas transport begins – a complex biological mechanism precisely coordinated between the circulatory and respiratory systems. Oxygen is introduced into the blood and distributed to each tissue and active cell. At the same time, carbon dioxide – a metabolic waste – must be rapidly collected for removal, maintaining a stable internal environment for the entire body.
Oxygen binds to hemoglobin
Oxygen dissolves in plasma and attaches to hemoglobin in red blood cells to form oxyhemoglobin. Each hemoglobin molecule carries up to four oxygen molecules, creating an efficient transport system that delivers oxygen to all necessary tissues through the sophisticated branching vascular system.
CO₂ metabolism and excretion
Carbon dioxide from cells is introduced into the blood in three forms: dissolved in plasma, bound to hemoglobin, or converted to bicarbonate ions by the enzyme carbonic anhydrase. When blood reaches the lungs, CO₂ is separated, diffuses into the alveoli, and is expelled through exhalation.
Lung Volumes and Capacities Explained
Lung capacity and volume reflect the body's respiratory capacity and are important for assessing respiratory health. Each breath is not simply about taking air in and out but also involves a series of sophisticated measurements showing the degree of expansion, elasticity, and efficiency of gas exchange in the lungs. These parameters vary with age, gender, body size, and level of training.
Tidal volume (TV)
The air you inhale and exhale normally averages about 500ml in adults.
Inspiratory reserve volume (IRV) and expiratory reserve volume (ERV)
IRV is the amount of air that can be inhaled after a normal inhalation; ERV is the amount of air that can be exhaled after a normal exhalation.
Total lung capacity (TLC) and functional residual capacity (FRC)
TLC is the air the lungs can hold after a maximal deep inspiration. FRC is the amount of air remaining after a normal exhalation – it plays a role in maintaining stable gas exchange even between breaths.
How Lung Function Is Measured
Lung function assessment is an essential step in diagnosing and monitoring respiratory diseases. Modern measurement techniques quantify breathing capacity and provide insight into gas exchange efficiency, lung elasticity, and respiratory muscle strength. Each index reflects a specific aspect of respiratory performance, from airflow to blood oxygenation.
Spirometry
Spirometry measures the volume of air inhaled and exhaled and the speed of airflow. FEV₁ and FVC help determine the degree of airway obstruction or restriction, aiding in the diagnosis of asthma, COPD, and pulmonary fibrosis.
Peak flow test
Peak flow measures the forceful rate at which air is expelled from the lungs. This portable device supports home asthma monitoring and assesses the risk of bronchospasm.
Arterial Blood Gas (ABG) Analysis
ABG directly analyzes the oxygen, CO₂, and pH concentration in arterial blood. The results reflect the efficiency of gas exchange and acid-base status, vital factors in treating respiratory failure and chronic diseases.
Factors Affecting Lung Function and How to Improve It
The environment, lifestyle, and biological factors deeply influence lung function. Each factor marks the ability to exchange gases, the elasticity of lung tissue, and the patency of the airways. Correctly identifying and proactively improving the influencing factors is the foundation for maintaining a healthy respiratory system and preventing lung function decline over time.
Air pollution and cigarette smoke
Fine dust particles, toxic gases, and cigarette smoke cause chronic inflammation, destroy the respiratory epithelium, and narrow the bronchioles. This continuous accumulation reduces ventilation and increases the risk of obstructive pulmonary disease.
Physical activity and deep breathing
Regular aerobic exercise increases vital capacity and improves alveolar ventilation. Deep breathing exercises increase lung elasticity and optimize gas exchange.
Nutrition and disease prevention
Diets rich in antioxidants protect lung tissue from free radical damage. Flu and pneumococcal vaccinations help prevent infections, the leading cause of sudden respiratory failure.
Conclusion
The lungs are the respiratory system's central organs, coordinating air flow and keeping life running smoothly. Every oxygen molecule that enters the body results from a precise chain of reactions, coordinating anatomical structures and sophisticated physiological activities.
Understanding lung function helps improve disease prevention and proactively maintain long-term respiratory health. All need to be seriously considered, from the mechanism of breathing and gas exchange to environmental factors.
Want to explore deeper? Check our guide on "lung structure and roles
Frequently Asked Questions (FAQs)
- What is the function of the lungs? – The lungs are responsible for gas exchange, delivering oxygen to the blood and removing carbon dioxide from the body, while maintaining pH balance and supporting energy metabolism at the cellular level.
- How much air can the lungs hold? – The total lung capacity of an average adult is about 6 liters, including the tidal volume, inspiratory reserve, expiratory reserve, and residual volume that cannot be exhaled.
- Where does gas exchange take place in the lungs? – Gas exchange occurs in the alveoli – microscopic structures with a dense network of capillaries, where oxygen and CO₂ diffuse through thin membranes into the circulatory system.
- How to improve lung function? – Regular aerobic exercise, avoiding exposure to dust and smoke, maintaining a diet rich in antioxidants, and vaccination against respiratory diseases are all measures to help the lungs function optimally.
- Why is measuring lung function important? – Measuring pulmonary function helps detect respiratory disorders early, monitor the progression of chronic lung disease, and adjust treatment methods according to specific physiological indicators.

